Originally published on the American Red Cross Southeastern Pennsylvania Region’s blog.

Most don’t know there is an American Red Cross Histocompatibility Laboratory right here in Philadelphia. It is 1 of 5 nationwide!
This laboratory provides a life-saving American Red Cross service for transplantation. The lab tests for the compatibility of a donor’s organ with the recipient of the organ. For example, those who want to donate a kidney are tested to find a recipient whose body will accept the kidney. This testing is called HLA typing. HLA typing is also used for matching bone marrow of a donor with someone who has a blood cancer, and to determine whether a platelet donation is a match with someone who has a clotting disorder and needs platelets.
The HLA typing process is complex and requires a special laboratory.
I am an American Red Cross Volunteer and Clinical Laboratory Scientist. I wanted to see this laboratory and understand HLA typing. I called Dr. Mary Philogene, Senior Director. She invited me to visit the laboratory and meet the technologists.
When I arrived, Dr. Philogene introduced me to Selina Taylor (pictured below), a histocompatibility certified technologist. Histocompatibility means finding compatibility among tissues. Selina has over 20 years of experience. She explained HLA is an acronym for Human Leukocyte Antigen. Human Leukocyte Antigens are found on every cell in our body, except red blood cells.

HLA typing and matching are more complicated than red blood cell ABO typing because there are over 15,000 HLA antigens with more than 22,000 subtypes. Each individual’s HLA type is a unique combination of these antigens and subtypes. There are thousands of HLA types. Finding the right match for a transplant can take months and even years.
Dr. Philogene led me into the laboratory where blood samples are received from New York, New Jersey, and Pennsylvania, and locally from Jefferson Medical Center, Dupont Children’s Hospital and Christiana Medical Center to name a few.
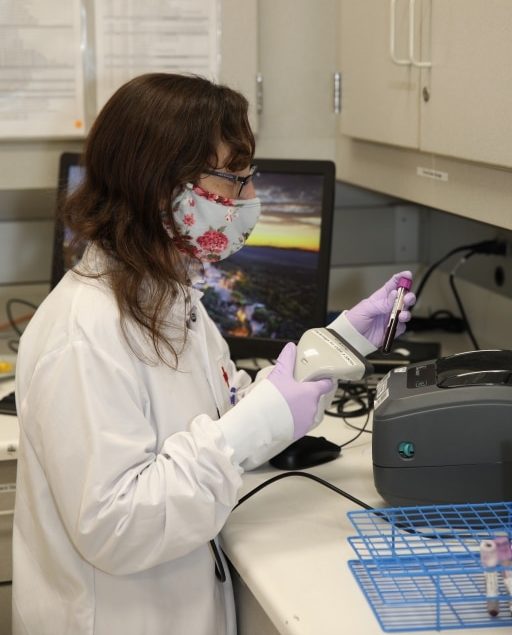
I met Jaclyn Connor (pictured below) who logs in information for each sample. Another technologist verifies each sample is correctly logged. Because patients and donors are only typed once, it’s critical to make sure each one is properly entered into the laboratory information system.
Next, the blood samples are sent to the laboratory for HLA typing. A process called DNA Sequencing is used to determine an individual’s HLA type.
Jessica Garbacz (pictured below) receives the blood samples. She places the samples into an instrument that extracts the DNA from blood and determines how much DNA is in each individual sample.
Then, Victoria Quann (pictured below) places the purified DNA into a PCR Thermocycler. This instrument increases the amount of DNA in each sample so it can be detected by the DNA Sequencing Analyzer.
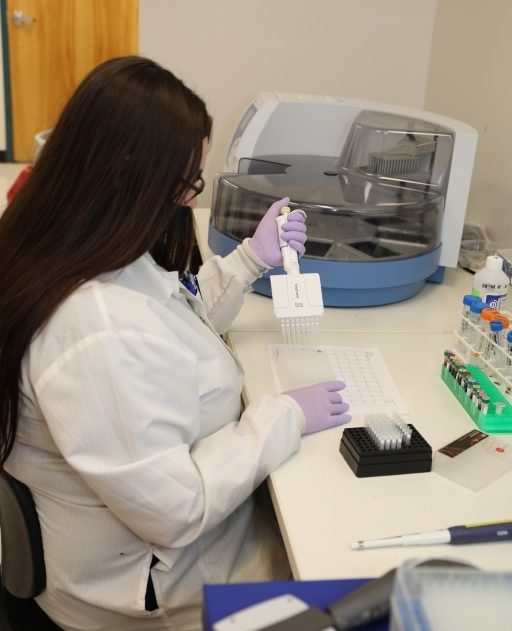
Selina Taylor (pictured below) prepares samples for DNA Sequencing by adding tiny droplets of each sample into a small plate with 96 wells, one for each sample.

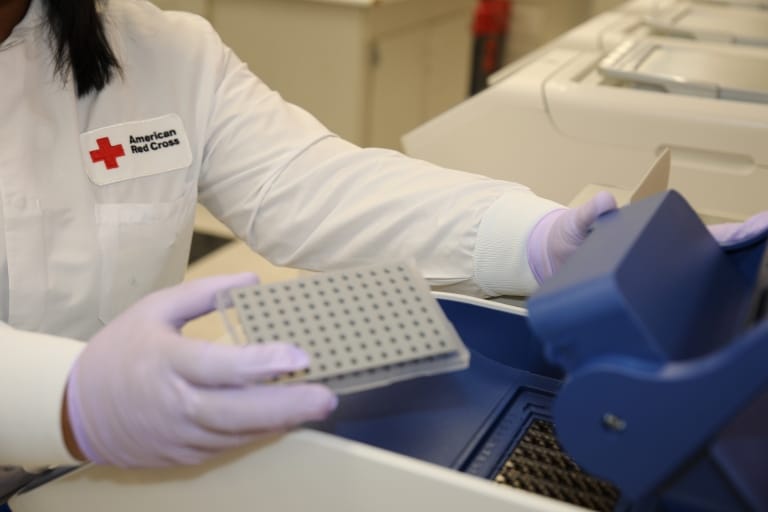
Victoria (pictured below) inserts this plate into the DNA Sequencing Analyzer. This analyzer produces a graph of each individual sample’s DNA sequence.

The graphs are sent to Alex Sum (pictured below) who analyzes them, identifying HLA type for donor or recipient.
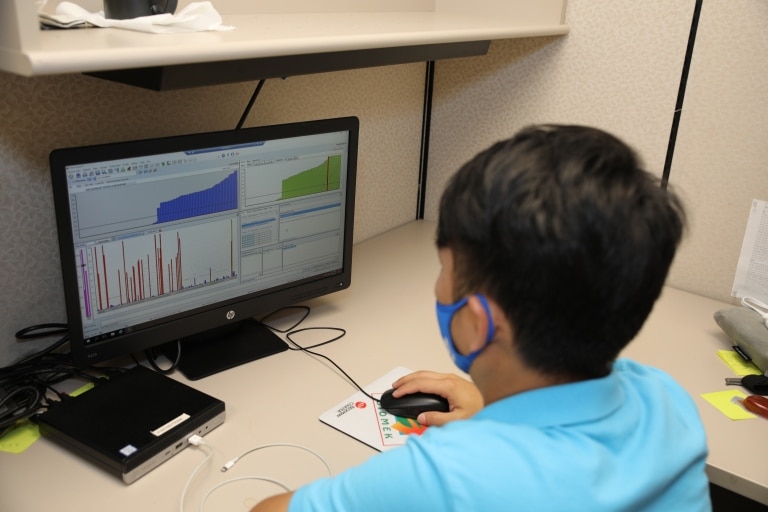
Eric Pimpinella (pictured below) is analyzing graphs from another DNA Sequencing that types platelet donors. Then he reviews reports with the HLA type before sending them to a hospital or a donor registry.

The success of a transplant is dependent on HLA typing by this Red Cross Laboratory. A look “behind the scenes” gave me an appreciation of the life-saving work by these dedicated people!
